Beyond the Common: Exploring Rare Types of Arthritis

Introduction
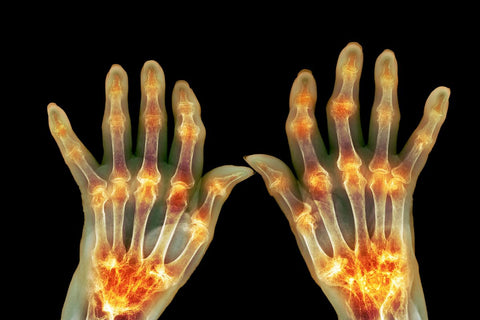
Arthritis is a common condition that affects the joints, causing pain, stiffness, and inflammation. It encompasses a range of disorders that involve inflammation in the joints, leading to symptoms like swelling, redness, warmth, and decreased range of motion. The most prevalent types are osteoarthritis and rheumatoid arthritis, but there are also rare forms that are less understood and often overlooked. These rare types can be challenging to diagnose and treat due to their complexity and limited research.
Importance of Understanding Rare Types
Understanding rare types of arthritis is crucial for several reasons. Firstly, it ensures that individuals with these conditions receive proper diagnosis and treatment, improving their quality of life. Secondly, research into rare types can lead to advancements in the overall understanding of arthritis, potentially benefiting those with more common forms as well. By shedding light on these lesser-known conditions, we can expand our knowledge and improve outcomes for all arthritis patients.
The purpose of this article is to raise awareness about rare types of arthritis, highlighting the importance of recognizing and addressing these less common conditions. By delving into the unique challenges faced by individuals with rare forms of arthritis, we aim to provide insight, support, and resources for both patients and healthcare professionals. Through education and advocacy, we can work towards a better understanding of arthritis as a whole, fostering improved care and outcomes for everyone affected by this diverse group of conditions.
Brief Explanation of Common Types
Arthritis comes in various forms, with osteoarthritis and rheumatoid arthritis being the most well-known. Osteoarthritis, often linked to aging or joint injury, involves the breakdown of cartilage in the joints, leading to pain and stiffness. On the other hand, rheumatoid arthritis is an autoimmune disorder where the body's immune system mistakenly attacks the joints, causing inflammation and damage.
These common types affect millions worldwide and are extensively studied and treated.
Prevalence and Impact
Arthritis is a prevalent condition, affecting people of all ages, genders, and backgrounds. It can have a significant impact on daily life, causing pain, reduced mobility, and decreased quality of life for many individuals. The economic burden of arthritis is substantial, with costs related to healthcare, lost productivity, and disability adding up. Recognizing the widespread impact of arthritis underscores the importance of research, education, and support for those affected.
Transition to Rare Types
As we move from the well-known common types to the rare forms of arthritis, we enter a realm that is less understood but equally important. Rare types like ankylosing spondylitis, systemic lupus erythematosus (SLE), or juvenile idiopathic arthritis present unique challenges due to their rarity and diverse manifestations. These conditions may require specialized care from healthcare providers with expertise in rare diseases.
Exploring these less common types, we can broaden our understanding of arthritis as a whole and improve outcomes for all patients, regardless of the specific type they have.

Understanding Rare Types of Arthritis
Definition and Classification
Rare types of arthritis encompass a diverse group of conditions that are less common than well-known forms like osteoarthritis and rheumatoid arthritis. These conditions often present unique symptoms and challenges, making them harder to diagnose and treat effectively. Examples of rare types include Mixed Connective Tissue Disease (MCTD), Reactive Arthritis (ReA), and Septic Arthritis (SA). Each of these conditions has distinct characteristics that set them apart from more prevalent forms of arthritis, requiring specialized care and attention.Factors Contributing to Rarity
Several factors contribute to the rarity of certain types of arthritis. These may include genetic predispositions, environmental triggers, or autoimmune mechanisms that are not fully understood. The complex interplay of these factors can lead to the development of rare forms of arthritis in a small percentage of the population. Limited research and awareness about these conditions also contribute to their rarity, as they may go undiagnosed or misdiagnosed, further adding to the challenge of managing these diseases effectively.
Challenges in Diagnosis and Treatment
Diagnosing and treating rare types of arthritis pose significant challenges for healthcare providers. The lack of awareness and specific diagnostic criteria for these conditions can result in delays in diagnosis and appropriate treatment. Additionally, the symptoms of rare arthritis types may overlap with other diseases, complicating the diagnostic process.
Treatment options for rare forms of arthritis are often limited, with healthcare professionals focusing on managing symptoms and improving quality of life rather than curing the condition outright. The complexity of these rare types requires a multidisciplinary approach involving rheumatologists, specialists, and other healthcare professionals to provide comprehensive care for individuals affected by these less common forms of arthritis.
Top 10 Rare Types of Arthritis
1. Ankylosing Spondylitis
Causes, Symptoms, and Diagnosis:
Ankylosing spondylitis (AS) is a chronic inflammatory condition that primarily affects the spine and sacroiliac joints (where the spine connects to the pelvis). This type of arthritis has a strong genetic component and is associated with the HLA-B27 gene. People with AS often experience intense back pain and stiffness, especially in the morning or after periods of inactivity.
Diagnosis of AS can be tricky, as symptoms may mimic those of other conditions. However, doctors may use a combination of physical exams, blood tests, and imaging techniques (such as X-rays and MRI scans) to confirm the diagnosis.
Treatment Options and Management Strategies:
While there is no cure for AS, various treatments can help manage symptoms and slow the progression of the disease. Non-steroidal anti-inflammatory drugs (NSAIDs) and exercise are often the first lines of defense. In more severe cases, biological therapies (like TNF inhibitors) and disease-modifying antirheumatic drugs (DMARDs) may be prescribed.
Regular exercise, maintaining good posture, and stopping smoking are also crucial for managing AS and preventing spinal fusion (a potential complication where the vertebrae fuse together).
2. Behçet's Disease
Overview and Symptoms:
Behçet's disease is a rare and complex autoimmune disorder that causes inflammation in various parts of the body. This condition is characterized by recurrent oral and genital ulcers, as well as potential involvement of the eyes, skin, joints, and other organs.
Symptoms can vary greatly among individuals, but may include mouth and genital sores, eye inflammation (uveitis), skin lesions, and joint pain or arthritis. Behçet's disease can also affect the digestive system, leading to abdominal pain and diarrhea.
Diagnosis and Treatment Approaches
Diagnosing Behçet's disease can be challenging due to its diverse symptoms and lack of a specific diagnostic test. Doctors often rely on a combination of clinical findings, medical history, and ruling out other conditions.
Treatment for Behçet's disease depends on the specific symptoms and severity of the condition. Corticosteroids, immunosuppressants, and biologic therapies are commonly used to manage inflammation and prevent flare-ups. Supportive care, such as topical treatments for mouth and genital ulcers, may also be necessary.
3. Reactive Arthritis
Causes and Triggers
Reactive arthritis, also known as Reiter's syndrome, is a type of arthritis that develops as a reaction to an infection, typically in the gastrointestinal or genitourinary tract. Common triggers include bacterial infections like Chlamydia, Salmonella, and Shigella.
The exact mechanism behind reactive arthritis is not fully understood, but it is believed to involve an abnormal immune response that leads to joint inflammation and other symptoms.
Symptoms and Complications
Reactive arthritis often presents with a triad of symptoms: arthritis (joint pain and swelling, typically affecting the knees, ankles, and feet), conjunctivitis (eye inflammation), and urethritis (inflammation of the urethra, causing pain during urination).
In addition to these symptoms, reactive arthritis can also cause skin lesions, low back pain, and inflammation in other parts of the body. If left untreated, it can lead to chronic joint damage and deformities.
4. Systemic Lupus Erythematosus (SLE)
Characteristics and Impact
Systemic lupus erythematosus (SLE) is a chronic autoimmune disorder that can affect virtually any organ or system in the body. It is characterized by periods of flare-ups and remissions, during which the immune system attacks the body's own tissues and organs.
SLE can cause a wide range of symptoms, including joint pain and swelling, fatigue, skin rashes, fever, and organ inflammation (such as in the kidneys, lungs, or heart). This unpredictable nature of SLE makes it a particularly challenging condition to manage.
Diagnosis and Management
Diagnosing SLE can be difficult due to its diverse symptoms and the fact that it mimics other conditions. Blood tests, such as the antinuclear antibody (ANA) test, can help detect the presence of autoantibodies, but a combination of clinical findings and diagnostic tests is often necessary.
Treatment for SLE aims to manage symptoms, prevent flare-ups, and minimize organ damage. Medications like corticosteroids, antimalarials, and immunosuppressants are commonly prescribed, along with supportive care and lifestyle modifications (such as stress management and sun protection).
5. Juvenile Idiopathic Arthritis (JIA)
Types and Manifestations
Juvenile idiopathic arthritis (JIA) is a group of autoimmune disorders that cause chronic joint inflammation in children and adolescents under the age of 16. JIA can be classified into several types, including oligoarticular (affecting four or fewer joints), polyarticular (affecting five or more joints), systemic (with fever and rash), and others.
In addition to joint pain, swelling, and stiffness, JIA can also cause growth abnormalities, eye inflammation (uveitis), and other systemic symptoms, depending on the type and severity of the condition.
Treatment Modalities
Early and aggressive treatment is crucial for managing JIA and preventing long-term joint damage and disability. Treatment strategies may include:
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Disease-modifying antirheumatic drugs (DMARDs)
- Biologic therapies (such as TNF inhibitors)
- Corticosteroids (for severe flare-ups)
- Physical and occupational therapy
-
Eye drops or other treatments for uveitis
Regular monitoring and a multidisciplinary approach involving pediatric rheumatologists, ophthalmologists, and other specialists are essential for optimal care and management of JIA.
6. Sjögren's Syndrome
Overview and Symptoms
Sjögren's syndrome is an autoimmune disorder that primarily affects the moisture-producing glands, leading to dry eyes and dry mouth. However, it can also cause inflammation and damage to other organs, including the joints, lungs, kidneys, and nervous system.
Common symptoms of Sjögren's syndrome include dry eyes (causing burning, grittiness, and blurred vision), dry mouth (which can lead to difficulty swallowing, dental problems, and increased risk of oral infections), joint pain and swelling, fatigue, and muscle aches.
Management and Prognosis
While there is no cure for Sjögren's syndrome, various treatments can help manage symptoms and prevent complications. Artificial tears and saliva substitutes can alleviate dry eyes and mouth, respectively. Medications like anti-inflammatory drugs, immunosuppressants, and biologic therapies may be prescribed to manage joint pain and other systemic manifestations.
Regular monitoring and a multidisciplinary approach involving rheumatologists, ophthalmologists, and dentists are essential for managing Sjögren's syndrome and preventing long-term complications, such as vision problems, dental issues, and lymphoma (a rare but potentially serious complication).
7. Gout
Causes and Risk Factors
Gout is a type of inflammatory arthritis caused by the buildup of uric acid crystals in the joints. This buildup can occur due to a variety of reasons, including genetic predisposition, high levels of purines (found in certain foods, like red meat and seafood), obesity, and certain medications or medical conditions.
While gout can affect anyone, certain risk factors increase the likelihood of developing this condition, such as being male, having a family history of gout, consuming a diet high in purines, being overweight or obese, and consuming excessive amounts of alcohol.
Treatment Strategies and Lifestyle Recommendations
During acute gout attacks, treatment focuses on reducing inflammation and managing pain. Non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and colchicine are commonly prescribed to alleviate symptoms.
Long-term management of gout involves lowering uric acid levels through medication (such as xanthine oxidase inhibitors or uricosuric agents) and lifestyle modifications. These modifications may include:
- Maintaining a healthy weight
- Limiting purine-rich foods (like red meat, seafood, and organ meats)
- Drinking plenty of fluids
- Limiting alcohol consumption
-
Exercising regularly
With proper treatment and lifestyle changes, it is possible to effectively manage gout and prevent future attacks and complications.
8. Polymyalgia Rheumatica
Symptoms and Diagnosis
Polymyalgia rheumatica (PMR) is an inflammatory condition that primarily affects the muscles surrounding the shoulders, hips, and neck. It typically occurs in individuals over the age of 50 and is characterized by severe muscle pain and stiffness, particularly in the morning or after periods of inactivity.
In addition to muscle pain and stiffness, people with PMR may also experience fatigue, fever, and weight loss. Diagnosis of PMR involves a thorough medical history, physical examination, and blood tests to check for elevated inflammatory markers (such as C-reactive protein and erythrocyte sedimentation rate).
Treatment Approaches
Treatment for PMR typically involves the use of low-dose corticosteroids (such as prednisone) to reduce inflammation and alleviate symptoms. The dosage is gradually tapered over time as the condition improves.
In some cases, additional medications like methotrexate or biologic therapies may be prescribed to help manage the condition and reduce the long-term use of corticosteroids. Physical therapy and exercise programs can also help improve muscle strength and flexibility.
Regular monitoring and follow-up with a rheumatologist are essential to ensure proper management of PMR and to detect any potential complications or associated conditions (such as giant cell arteritis, which can occur in some cases).
9. Psoriatic Arthritis
Relationship with Psoriasis
Psoriatic arthritis is a type of inflammatory arthritis that affects some individuals with psoriasis, a chronic autoimmune skin condition characterized by raised, red, and scaly patches. It is estimated that up to 30% of people with psoriasis will develop psoriatic arthritis.
The exact relationship between psoriasis and psoriatic arthritis is not fully understood, but it is believed to involve a complex interplay between genetic and environmental factors that trigger an abnormal immune response.
Symptoms and Treatment Options
Psoriatic arthritis can affect various joints, including the small joints of the hands and feet, as well as the spine and larger joints like the knees and hips. Common symptoms include joint pain, swelling, stiffness, and reduced range of motion. In some cases, it can also cause nail changes and inflammation of the eyes or other organs.
Treatment for psoriatic arthritis typically involves a combination of medications (such as non-steroidal anti-inflammatory drugs, disease-modifying antirheumatic drugs, and biologic therapies), physical therapy, and lifestyle modifications (like maintaining a healthy weight and managing stress).
Additionally, topical treatments and phototherapy may be used to manage the skin manifestations of psoriasis. A multidisciplinary approach involving rheumatologists, dermatologists, and other specialists is often necessary for optimal management of psoriatic arthritis.
10. Mixed Connective Tissue Disease (MCTD)
Features and Diagnosis
Mixed connective tissue disease (MCTD) is a rare autoimmune disorder that exhibits features of three other connective tissue diseases: systemic lupus erythematosus (SLE), scleroderma (systemic sclerosis), and polymyositis (an inflammatory muscle disease).
MCTD is characterized by a combination of symptoms, including joint pain and swelling, Raynaud's phenomenon (a condition that causes discoloration and numbness in the fingers and toes due to poor circulation), muscle weakness and inflammation, and other systemic manifestations.
Diagnosis of MCTD can be challenging, as it shares similarities with other connective tissue diseases. Blood tests for specific autoantibodies (such as anti-U1 RNP antibodies) and a combination of clinical findings are often used to confirm the diagnosis.
Treatment and Prognosis
Treatment for MCTD aims to manage symptoms, reduce inflammation, and prevent organ damage. Medications commonly used include corticosteroids, immunosuppressants, and biologic therapies (like TNF inhibitors or rituximab).
In addition to medication, lifestyle modifications (such as quitting smoking, staying physically active, and protecting the skin from sun exposure) can also help manage symptoms and improve overall well-being.
While MCTD is a chronic condition, early and aggressive treatment can help slow disease progression and improve long-term outcomes. Regular monitoring and a multidisciplinary approach involving rheumatologists, dermatologists, and other specialists are essential for optimal management of MCTD.
These rare types of arthritis may be less well-known, but they provide a glimpse into the fascinating and complex world of autoimmune and inflammatory conditions. By raising awareness and understanding of these conditions, we can work towards better diagnosis, treatment, and support for those affected.

Coping with Rare Arthritis
Psychological Impact of Rare Arthritis
Dealing with a rare form of arthritis can take a toll on your mental well-being. The uncertainty, challenges in diagnosis and treatment, and feelings of isolation can all contribute to increased stress, anxiety, and even depression. It's important to acknowledge these emotional struggles and seek support when needed. Remember, it's okay to feel overwhelmed at times, but reaching out to loved ones, joining support groups, or speaking to a mental health professional can help you navigate the psychological impact of living with a rare arthritis condition.
Support Systems and Resources
Building a strong support system is crucial when coping with rare arthritis. Surround yourself with understanding friends and family members who can offer emotional support and practical help when needed. Additionally, consider joining online or in-person support groups specifically for individuals with rare forms of arthritis.
These communities can provide valuable insights, shared experiences, and a sense of belonging that can make a significant difference in your journey. Don't hesitate to explore resources offered by patient advocacy organizations or healthcare providers specializing in rare diseases for additional support.
Lifestyle Adjustments for Better Quality of Life
Making lifestyle adjustments can greatly improve your quality of life while living with a rare form of arthritis. Focus on maintaining a healthy diet rich in anti-inflammatory foods like fruits, vegetables, whole grains, and omega-3 fatty acids to help manage symptoms. Regular exercise tailored to your abilities can strengthen muscles, improve flexibility, and reduce pain.
Prioritize stress management techniques such as mindfulness, meditation, or yoga to promote relaxation and overall well-being. Remember to pace yourself, listen to your body, and communicate openly with your healthcare team to ensure you're receiving the best possible care for your unique needs.





